Dr. Frankel’s Case of the Week:
Pseudotumor Cerebri

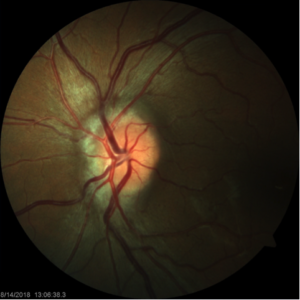
A 36-year-old female presented to our office with a complaint of headaches and a “strange sound in her ears”. She described this as hearing her heart murmur. He has had no recent weight gain and no episodes of vision loss. She is taking an oral contraceptive, medication for hyperactive bladder and hypertension. Her visual acuity was 20/20 OU with no APD noted by the technician. Her confrontation visual field was full to careful finger counting and her EOMs were FULL. Her IOP was 15 mmHg OU. Her anterior segment exam was significant for early dry eye changes. Her posterior exam revealed elevated nasal optic nerve heads with blurring of the disc margin OU and mild obscuration of the vessels. Her right eye had a peripapillary hemorrhage and suprotemporal paton’s lines. The retina was flat and intact 360 with no holes, tears or retinal detachments. Visual fields revealed arcuate defects OU.
She was sent for MRI of the brain and orbits and lumbar puncture with composition and opening pressure and will be following up with neuro-ophthalmology
Pseudotumor cerebri is a disease entity in which patients present with signs and symptoms of increased intracranial pressure of unknown cause. It most commonly effects obese women of childbearing age.
The clinical symptoms most commonly seen in pseudotumor are headaches, transient episode of vision loss, pulsatile tinnitus, and diplopia. Upon examination, papilledema is the hallmark sign of pseudotumor cerebri.
The pathophysiology remains unclear but multiple hypotheses have been suggested. Cerebral edema was one of the earliest proposed pathological mechanisms for pseudotumor cerebri. However, it was quickly criticized as the elevated ICP was not associated with altered levels of alertness, cognitive impairments, or neurologic findings typically seen with cerebral edema.


A current hypothesis that has received substantial interest involves stenosis of the distal portion of the transverse cerebral sinuses. A study performed by Farb et al demonstrated evidence of narrowing in the transverse sinus among 29 patients with pseudotumor; whereas none of the 59 control subjects had these findings.
Another suggestion is that an increase in intraabdominal pressure, secondary to obesity, causes increased cardiac filling pressure which impedes venous return from the brain and subsequently leads to an elevated intracranial venous pressure. However, this hypothesis is unable to explain its presence among the non-obese population group.
Other studies have suggested a role of vitamin A in the pathogenesis based on elevated serum and CSF vitamin A, retinol, and retinol binding protein levels reported in patients with pseudotumor. The significance of these findings remains unclear.
The goal of treatment is to alleviate symptoms and preserve vision. All obese patients should be encouraged to lose weight. Patients who are obese or overweight, weight loss of about 5-10% has been found to improve symptoms and signs. Medical therapy is usually considered among patients with mild to moderate disease.
Among the options available, acetazolamide, a carbonic anhydrase inhibitors, is believed to reduce the rate of CSF production and is the first-line medical treatment for IIH. Topiramate and/or furosamide can also be used. Although steroids were previously recommended, their use is no longer suggested due to their undesired side-effects (mainly weight gain) and the rebound intracranial hypertension following its discontinuation.
Surgical management is the option of choice among patients with refractory headaches or more severe or progressive visual field loss when all other options have failed. The two most used procedures are CSF shunt and optic nerve sheath fenestration. The choice of the procedure is based on patients’ signs and symptoms.
To have your eyes checked for any major ocular diseases, make an appointment with Dr. Frankel. Give our office a call or simply schedule an appointment via ZocDoc.
On social media? Like us on Facebook & Follow us on Instagram
