Dr. Frankel’s Case of the Week: Hydrops
A 37 y.o. female presents to the clinic for pain, photophobia, itching and tearing for 2 days. The patient went to the ER the day before and was told that she had an abrasion. She was given Ciprofloxacin QID and told to follow up with ophthalmology. She had been experiencing itching and discomfort for a few months prior to this episode, which resulted in her rubbing the eye incessantly. She was seen by two outside ophthalmologists 2 months prior to our encounter for this itching and discomfort. She was instructed at that time to start using artificial tears and the condition will be monitored.
Entering visual acuity was 20/30 OD and HM OS. EOMs were FULL and confrontation fields were full to careful finger counting. Her pupil was unable to be visualized OS, and OD was reactive with no APD by reverse. Anterior segment examination revealed an unremarkable examination OD, and a corneal ectasia of about 60% of the cornea OS. There was significant white stromal edema in a somewhat linear pattern with overlying microcystic edema. There was no epithelial defect. Her current spectacle RX was OS: -3.50-2.00×180 OS:-2.75-1.50×70; which was not indicative of keratoconus. She was told to discontinue using Ciprofloxacin and start Muro 128 ointment and drops QID as well as Prednisolone gtts QID OS.
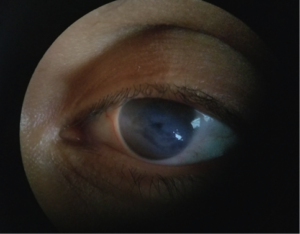

She returned the office a few days later for follow up and admitted to good compliance with her drops, but admitted to rubbing the eye often since the last visit. She had no change in her visual aquity, and her anterior segment examination revealed worsening of her hydrops. I discussed that this is causing the damage to her eye and that we should get a cornea specialist involved in her care at this point. She was advised to continue her current medical regimen as well as Pazeo QD-BID to assist in reducing the desire to rub the eye.
Acute corneal hydrops from eye rubbing secondary to a vernal or atopic keratoconjunctivitis is not commonly seen in practice. Corneal hydrops is characterized by stromal edema due to leakage of aqueous humor through a tear in Descemet’s membrane. This can lead to corneal scarring when the edema results in a break in Bowman’s membrane. Generally, the resulting corneal edema precludes one’s ability to visualize this structural damage. Ancillary tests such as anterior segment OCT and ultrasound biomicroscopy aid in gauging the extent of damage on the tissues. In this particular case, there was a break made to Descemet’s membrane from the patient rubbing her eye. The majority of these cases are resolved with hypertonic and steroid drops. Bandage soft contact lenses can also be utilized when corneal bullae are present. In some circumstances, there is too much damage to the posterior structures of the cornea and the patient is in need of surgical intervention. Surgeries can include DSEK, DMEK or even PKP.
To have your eyes checked for any major ocular diseases, make an appointment with Dr. Frankel. Give our office a call or simply schedule an appointment via ZocDoc.
On social media? Like us on Facebook & Follow us on Instagram
