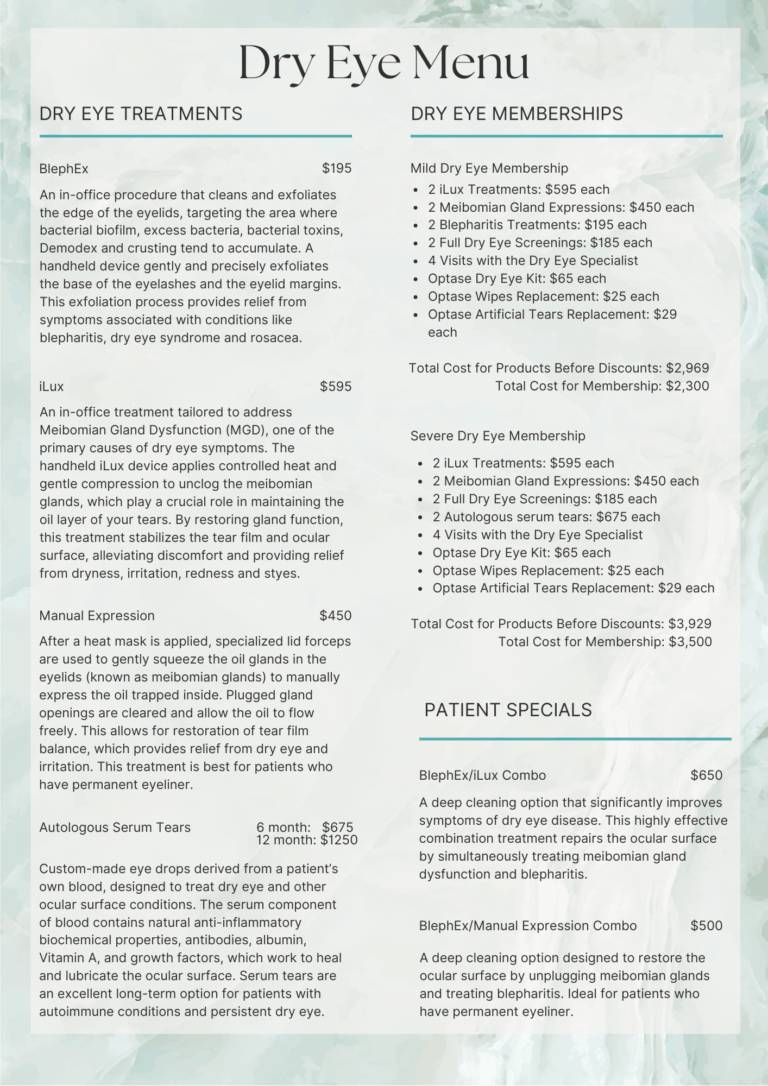
Why Aren’t Effective Dry Eye Treatments Covered by Insurance?
Dry eye is a real medical condition that affects your comfort, vision, and quality of life. However, the most effective treatments are not covered by insurance. Here’s why:
- Insurance covers “necessary” treatments, not “comfort” care.
- Insurance plans only cover what they consider medically necessary to treat disease. Even though dry eye can feel awful or be diagnosed as severe, insurance carriers see it as a chronic, uncomfortable, non-urgent condition, similar to acne or allergy care. Even though your doctor may tell you that treatment is “medically recommended,” that is not the same thing as what your insurance qualifies as “medically necessary.” Your doctor has no power or authority to dictate to your insurance company what is medically necessary for dry eye diagnosis and care. It does not matter if you are diagnosed with severe ocular surface disease; there is no letter or appeal processes that any medical provider can send to your insurance company to get something covered for you. Additionally, dry eye cannot be billed to vision insurance, which is designed only to help cover the costs of exams for prescriptions for glasses/contact lenses and materials.
- Advanced testing and treatments are considered by medical insurance companies to be elective and innovative management:
- Dry eye panel testing
- IPL (Intense Pulsed Light)
- RF (Radiofrequency)
- DMSt (Dynamic Muscle Stimulation)
- iLux (gland treatments)
- BlephEx (eyelid exfoliation)
- Manual gland expression
- Scleral lenses for dry eye management
- Autologous serum tears
- Things insurance may cover with copayments/coinsurance/deductibles:
- Medical exams and follow-up care.
- Prescription eye drops (with prior authorization). If a patient has not had success with other dry eye therapies, such as artificial tears.
- In-office punctal plug insertion, if a patient has not had success with other dry eye therapies, such as artificial tears.
- Amniotic membrane grafts, if a patient has severe ocular surface disease.

Your medical providers have no control over your prescription insurance coverage. Most of the time, when prescription eye drops are sent to your pharmacy, insurance providers will request that generics be sent instead. Copayments for branded prescription eye drops can be very high, and your physician cannot change that. Often, patients see advertisements for Restasis/Xiidra/Cequa/Veyve/Xdemvy/Miebo/Tyrvaya. NONE of these branded dry eye medications are available in a generic equivalent form except Restasis, which comes in generic cyclosporine. Additionally, ongoing treatments to restore gland function or reduce inflammation are not part of your benefits.
- We’re here to help you get the care you need:
- Clear pricing up front
- Bundled treatment plans and packages to save you money
- Acceptance of HSA/FSA
- Financing options with Care Credit
We believe in treating the root cause of your dry eye, not just masking the symptoms.
Have questions? Just ask. We’re happy to walk you through your options.